Gastric Sleeve (Sleeve Gastrectomy)
What is a Gastric Sleeve?
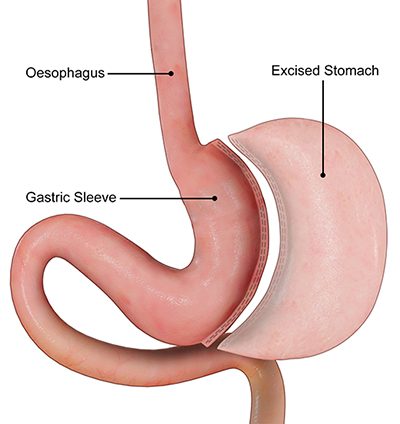
Gastric sleeve, also referred to as vertical sleeve, sleeve gastrectomy or tube gastrectomy, is a combined restrictive and metabolic type of weight loss surgery.
The size of the stomach is reduced with 75% of the stomach removed and thereby limiting/restricting its storage capacity.
Another mechanism of weight loss in this surgery is achieved through hormonal changes in the gut which occurs via:
- removal of (most of) the section of the stomach that produces hunger hormones
- and increased speed of food being delivered to the downstream part of small bowel
The changes to the gut hormone profile leads to:
- suppression of appetite
- upregulation of internal body processes that cause energy expenditure
- reduction in conversion of calories to fat
- more effective regulation of blood sugar levels.
The excess weight loss is expected to be around 60-70%. *
* Individual results may vary. Refer to our disclaimer
Why should you have weight loss surgery?
- It is the only treatment that is proven to be effective and sustainable for weight loss in the long term
- Lowers the risk of developing obesity-associated cancers
- Type 2 diabetes and many other obesity-associated diseases are often prevented, improved or cured
- Improvement in fertility (Especially in those with Polycystic Ovarian Syndrome)
- Allows you to live a longer, happier and healthier life!
* At Melbourne Weight Loss Centre, we provide personalised treatments that are tailored to your individual needs and your existing medical conditions.
Why choose to have a Gastric Sleeve?
The sleeve gastrectomy is the most common bariatric procedure carried out in Australia in recent years. This is mainly due to the greater efficacy for weight loss and higher rate of resolution of obesity-related health conditions (such as diabetes and high cholesterol) when compared to gastric banding. This is achieved through the metabolic/hormonal component of the operation which is absent in gastric banding. When compared to a gastric bypass, this procedure may have lower potential side-effects in the long-term including vitamin deficiencies and internal hernia.
Who is best suited to a Gastric Sleeve?
- Patients who desire greater weight loss than what is achieved with gastric banding
- Patients who are not motivated enough to stick with the diet required for gastric banding
- Patients who are looking for a less complex operation than a gastric bypass
- Patients with type 2 diabetes, high cholesterol, high blood pressure, osteoarthritis, and obstructive sleep apnoea
- Patients with fertility issues and wants to lose weight (ie. To improve chances of a pregnancy with or without IVF)
- Patients with Polycystic ovarian syndrome
Indications for Gastric Sleeve Surgery
Gastric sleeve is indicated for morbidly obese individuals with the following criteria:
- BMI is ≥ 40
- BMI is 35-39.9 with at least one or more associated co-morbidities such as type 2 diabetes, high blood pressure, high cholesterol level, heartburn, joint problems, breathing problems (obstructive sleep apnoea), etc…
- BMI is 30-34.9 with uncontrolled or poorly controlled type 2 diabetes with multiple anti-diabetic medications
* Please remember this is a guide only (rather than absolute indications for surgery) and it should be used as an educational reference. The information provided does not replace a medical consultation from the healthcare professional. An individual’s suitability for surgery should be assessed by an appropriately trained doctor on a case by case basis.
Advantages of Gastric Sleeve Surgery
The advantages of gastric sleeve include:
- Reduction in stomach size allowing for better satiety control
- Reduction in hunger hormones (Ghrelin) allowing for suppression of appetite
- Better weight loss efficacy than gastric band (in general)
- Higher rate of resolution (or improvement) of obesity-related conditions than gastric band
- Less follow-up visits than gastric band and gastric bypass overall
- Likely lower long-term complications than gastric bypass (such as vitamin deficiencies, internal hernia and others)
- No implant device in the body
Disadvantages of Gastric Sleeve Surgery
- Non-reversible
- Higher early complication rate than gastric band (ie. staple line leak)
- Risk of heartburn
- Lower diabetes remission rate than gastric bypass (but higher than gastric band)
Risks and Complications of Gastric Sleeve Surgery
As with any surgery, there is potential risk for complications to occur following a gastric sleeve, but they are considered to be relatively uncommon in the surgical literature. The immediate/early complications include:
- Internal bleeding
- Wound infection
- Blood clots in the legs or lungs
- Narrowing of the stomach tube
- Staple line leak
The main risk of late complication associated with this procedure is heartburn/reflux oesophagitis.
Gastric Sleeve Procedure
The procedure is performed laparoscopically (key-hole surgery) under general anaesthesia. The surgeon makes 5 small incisions in the abdominal wall through which a camera and surgical instruments can be inserted into. About 75-80% of the stomach is removed by a stapling/cutting device to create a thin tube-shaped stomach. If there is weakness in the diaphragmatic muscles around the top of the stomach or herniation of part of the stomach into the chest, this will be corrected and repaired during the same operation tom prevent heartburn/reflux. The resected stomach is then removed via one of the key-hole incisions at the end of the procedure.
Post-operative care for Gastric Sleeve
After the surgery, you will likely be staying in the hospital for about 2-4 days. Your doctor will prescribe pain-killers and anti-nausea medications to keep you comfortable following the procedure. Your nurse will help you to move at the earliest after the surgery to prevent blood clots, respiratory problems and bedsores. The swelling in your stomach after the operation can make it difficult to drink in the first few days which is a normal process. However, it is important to remember to sip on fluids throughout the day to avoid dehydration (especially in the first 1-2 weeks).
You will be kept on a liquid diet for the first 2 weeks post-op and then transition to puree diet and then soft diet at every 2 weeks afterwards. Your surgeon or dietician will give you a specific diet plan and instructions to follow after the surgery. You will be advised to take medication to reduce the amount of acid produced by your stomach for the first 3 months. You will also need to start taking multi-vitamins which will continue for life.
