Anti-reflux Surgery
What is Anti-reflux Surgery?
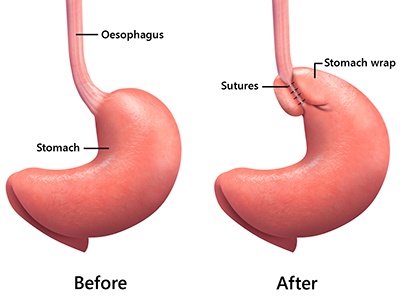
Anti-reflux surgery is a procedure used to treat gastro-oesophageal reflux disease (GORD). Typically, this would usually involve in repair of the hiatus hernia and creation of a fundoplication wrap which is a stomach wrap around the lower oesophagus to prevent reflux.
What is acid reflux or GORD?
Acid reflux, also called gastro-oesophageal reflux disease (GORD), is a condition where the stomach contents (food or liquid mixed with stomach acid) rise up from the stomach into the oesophagus (a tube that carries food from the mouth to the stomach).
Normally the stomach contents do not usually enter the oesophagus. This is due to a number of anatomical and physiological factors that contribute to the overall anti-reflux mechanism. One of these is constriction of the lower oesophageal sphincter (LES) which is a ring of muscle fibres that surrounds the lowest end of the oesophagus where it joins the stomach. LES acts like a valve between the oesophagus and stomach preventing food from moving backward into the oesophagus. However in patients with acid reflux, stomach content travels back into the oesophagus because of a weakened or relaxed LES.
Causes of acid reflux/GORD
The cause of GORD is thought to be due to a number of factors including aging, genetics, obesity, smoking, certain medications (eg, aspirin, ibuprofen), and presence of a hiatus hernia.
Symptoms of acid reflux/GORD
Heartburn is usually the main symptom of GORD; a burning-type of pain in the lower part of the mid-chest, behind the breast bone which may improve or resolve with antacid medications. Typically, it can be triggered by certain food and drinks such as tomatoes, citrus, mint, garlic, onions, fatty or spicy food, chocolate, alcohol, and carbonated and caffeinated drinks. Symptoms can also be position related which are worse when laying flat (particular at night in bed). There are also a number of other symptoms associated with GORD such as sore throat, hoarse voice, a bitter or sour taste in the mouth, dental erosions, dry cough or wheezing, regurgitation of food (bringing food back up into the mouth) and pain/trouble in swallowing. Rarely, aspiration of stomach contents into the chest can occur, resulting in pneumonia (chest infection).
Complications of acid reflux/GORD
Chronic acid (or bile) exposure to the oesophagus can lead to serious complications over time including:
- Reflux oesophagitis (inflammation of lower oesophagus)
- Barrett’s oesophagus (pre-cancerous condition of oesophagus)
- Oesophageal cancer
Tests/Investigations
There are several tests that may be performed to confirm or exclude the diagnosis of acid reflux and other associated conditions. These investigations include:
- Gastroscopy: This test allows the doctor to examine the inside of the patient’s oesophagus, stomach, and upper portions of the small intestine using an instrument called an endoscope which is a long, thin flexible lighted tube with a built-in camera.
- Barium swallow/meal: These are diagnostic x-rays in which barium is used to diagnose abnormalities of the digestive tract such as hiatus hernia, oesophageal dysmotility, reflux, and delayed gastric emptying. You are asked to swallow a liquid that contains barium and then barium-soaked bread to demonstrate the transit of liquid and solid in your oesophagus. Sequential x-rays are taken of you straight after you have swallowed.
- Oesophageal manometry: It is a test used to assess the contractions of your oesophagus when you are swallowing which will help your surgeon determine the type of stomach wrap to create for you in the operation. In addition, it will also detect any abnormalities in the function of the lower oesophageal sphincter. The investigation generally takes 15-20mins which involves in the insertion of a thin tube through your nose into your oesophagus and stomach to measure the pressures in these regions. You will be asked to lay on your left and swallow some liquids during which pressure recordings will be taken.
- 24-hour pH monitoring: In this procedure, a tube will be inserted through the nose into the oesophagus and positioned above the LES. The tip of the tube contains a sensor which can measure the pH of the acid content refluxed into oesophagus. A recorder, strap-like device that can be worn on wrist, will be connected to record the pH of the acid content. The tube will be left in place for 24 hours. Patients can also go back home and perform their regular activities and can record the pH of the acid content when they experience the symptoms. On the next day the recorder will be connected to a computer and the data will be analysed.
- Bravo PH Capsule: It is a new method of measuring acid exposure in the oesophagus. A small wireless capsule is introduced into the oesophagus by a tube through the nose or mouth under direct vision with an endoscope. The tube is removed after the capsule is attached to the lining of the oesophagus. The pH sensor transmits signals to a computer which collects the data about the acid exposure over the usual 24 hours. The capsule detaches from the oesophagus with time and is passed in the stool.
- Impedance study: This test is performed together with the 24-hour pH monitoring using a different type of probe which is inserted through the nose with the tip of the probe in the lower oesophagus. The sensor is able to detect the height of retrograde flow (backflow) of liquid, semi-solid or gas back up into the oesophagus.
Treatment
Antacids are over-the-counter medicines that provide temporarily relief to heartburn or indigestion by neutralising acid in the stomach. Other medications such as proton pump inhibitors and H2 antagonists may be prescribed by your GP to reduce the production of acid in the stomach.
Anti-reflux Surgery may be recommended in the following situations:
- Inadequate/partial response to treatment with maximal anti-acid medication
- Failed optimal medical treatment
- Unwilling to take life-long medication
- Non-compliant with medication
- Complications of reflux disease (such as oesophagitis, Barrett’s oesophagus, bleeding/anaemia/ulceration/narrowing due to chronic reflux oesophagitis, respiratory/upper airway symptoms, and aspiration pneumonia)
Surgical Procedure
The operation is performed laparoscopically (key-hole surgery) with the patient under general anaesthesia. The surgeon makes 5 small incisions in the abdominal wall through which a camera and surgical instruments can be inserted into.
The first stage of the procedure is the repair of the hiatus hernia which is often associated with reflux disease. Part of the stomach that has moved up into the chest cavity will be pulled back down into the abdomen. The upper stomach and lower oesophagus is dissected away from the surrounding tissue so that they are freely mobilised down into the abdomen without tension.
The hole in the diaphragm (called the hiatus) through which the oesophagus passes is widened in a hiatus hernia. This is partially closed or tightened with sutures so that the hole only permits the oesophagus through. Rarely, an absorbable mesh may be placed around this repair in a very large hiatus hernia or re-do operation which may reduce the risk of recurrence.
The upper part of the stomach (called the fundus) is then partially wrapped and secured around the lower oesophagus with sutures. This manoeuvre is called fundoplication which serves to re-create the valve effect that contributes to the anti-reflux mechanisms.
Risks /Complications of Procedure
Specific side-effect and complications for this operation include:
- Internal bleeding (due to injury to vessels or spleen)
- Infection (including pneumonia)
- Injury to stomach or oesophagus causing perforation
- Swallowing difficulties (due to stomach wrap being too tight)
- Gas-Bloat syndrome (a variable side-effect as a consequence of the stomach wrap)
