Gastric Bypass
What is a Gastric Bypass?
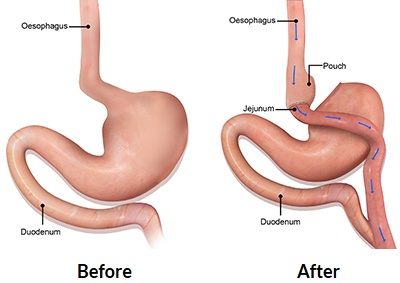
Gastric Bypass, also known as Roux-en-Y Gastric Bypass, is primarily a combined restrictive and metabolic weight loss procedure with a mildly malabsorptive component. The surgery involves in creating a small pouch at the top of the stomach and bypassing the flow of food away from the first part of the small intestine and directly into the middle part of the small intestine. The weight loss effect is primarily achieved through:
- restriction in the amount of food stored in the newly-created small stomach pouch
- changes in gut hormonal profile (which occur as a result of diversion of food away from the first part of the small bowel)
Additionally, there is a small, limiting effect on the absorption of food.
The excess weight loss is expected to be around 65-75%. *
* Individual results may vary. Refer to our disclaimer
Why should you have weight loss surgery?
- It is the only treatment that is proven to be effective and sustainable for weight loss in the long term
- Lowers the risk of developing obesity-associated cancers
- Type 2 diabetes and many other obesity-associated diseases are often prevented, improved or cured
- Improvement in fertility (Especially in those with Polycystic Ovarian Syndrome)
- Allows you to live a longer, happier and healthier life!
* At Melbourne Weight Loss Centre, we provide personalised treatments that are tailored to your individual needs and your existing medical conditions.
Why choose to have a Gastric Bypass?
Roux-en-y Gastric Bypass has been considered by some as the “Gold standard” of bariatric procedure which accounts for its enduring popularity in many parts of the world since it was first performed in 1967. Besides a greater efficacy in weight loss, the metabolic/hormonal component of the procedure has a better chance of normalising the blood sugar level in type 2 diabetic patients when compared to the other weight loss procedures. It is also the procedure of choice for those with bad concurrent heartburn/reflux disease.
Who is best suited to a Gastric Bypass?
- Patients who desire greater and more durable weight loss, but can accept potentially higher risk of long-term side-effects (such as vitamin deficiencies)
- Patients who want a reversible procedure
- Patients who have poorly-controlled or uncontrolled diabetes and want a better chance at a cure for it
- Patients with bad reflux/heartburn
- Patients who had failed previous weight loss procedures (such as gastric banding or gastric sleeve)
Indications for Gastric Bypass
Gastric Bypass surgery is indicated for morbidly obese individuals with the following criteria:
- BMI is ≥ 40
- BMI is 35-39.9 with at least one or more associated co-morbidities such as type 2 diabetes, high blood pressure, high cholesterol level, heartburn, joint problems, breathing problems (obstructive sleep apnoea), etc…
- BMI is 30-34.9 with uncontrolled or poorly controlled type 2 diabetes with multiple anti-diabetic medications
* Please remember this is a guide only (rather than absolute indications for surgery) and it should be used as an educational reference. The information provided does not replace a medical consultation from the healthcare professional. An individual’s suitability for surgery should be assessed by an appropriately trained doctor on a case by case basis.
Advantages of Gastric Bypass
The advantages of gastric bypass include:
- Better weight loss efficacy than gastric band and sleeve gastrectomy
- Higher rate of resolution (or improvement) of obesity-related conditions
- Reversible
- It is an anti-reflux operation and is thus most suitable for those with bad reflux/heartburn
- It may be better for uncontrolled or poorly controlled type II diabetes
- No implant device in the body
Disadvantages of Gastric Bypass
- Technically more complex than gastric banding or a sleeve
- Potentially greater side-effects in the long-term (such as dumping syndrome, stomal ulcer and internal hernia) compared to gastric sleeve
- Potential for vitamin deficiencies (particularly with iron, B12, calcium and folate) which requires regular monitoring
- Requires strict adherence to life-long vitamin/mineral supplementation and compliance with dietary recommendations
- Longer follow-up requirements (more doctor’s visits) compared to gastric sleeve
Risks and Complications of Gastric Bypass
As with any surgery, there are potential risks that are associated with a gastric bypass, but the complication rates are relatively low according to the literature in recent publications. The immediate/early complications include:
- Internal bleeding
- Infection
- Blood clots in legs or lungs
- Leaks along staple lines or joints between stomach to small intestine or small intestine to small intestine
However, the procedure is associated with potential risk of late complications such as:
- Dumping syndrome (leading to abdominal cramping, bloating, diarrhoea, flushing, sweating and palpitations)
- Narrowing of the joint between stomach and small intestine
- Ulceration at the joint between stomach and small intestine
- Internal hernia causing bowel obstruction
- Protein malnutrition/vitamin deficiencies
Gastric Bypass Procedure
Gastric bypass surgery is performed laparoscopically (key-hole surgery) under general anaesthesia. The surgeon makes 5 small incisions in the abdominal wall through which a camera and surgical instruments can be inserted into.
The first stage of the surgery involves in reducing the amount of food that can be stored in the stomach to reduce your calorie intake. This is achieved by creating a small stomach pouch below the oesophagus using a stapler/cutting device.
The second stage involves in construction of a bypass for food to flow from the new created stomach pouch to the lower segments of the small intestine.
After division of the upper segment from the lower segment of the small intestine, the lower segment (which is often referred to as the “Roux limb”) is then attached to the stomach pouch. The upper section of the small intestine which carries bile and digestive juices from the liver, pancreas and the remaining portion of the stomach is then joined to the lower end of the Roux limb. Below this joint is where food can mix with the digestive enzymes and this last segment of bowel is often referred to as the “Common limb”.
Post-operative Care for Gastric Bypass
After the surgery, you will typically be staying in the hospital for about 3-4 days. Your doctor will prescribe pain-killers and anti-nausea medications to keep you comfortable following the procedure. Your nurse will help you to move at the earliest after the surgery to prevent blood clots, respiratory problems and bedsores. The swelling in your stomach after the operation can sometimes make it difficult to drink which is a normal process. However, it is important to remember to sip water throughout the day to avoid dehydration (especially in the first 1-2 weeks).
You will be kept on a liquid diet for the first 1-2 weeks post-op and then, depending on your progress of recovery, transition to puree diet and then soft diet at every 1-2 weeks afterwards. Your surgeon or dietician will give you a specific diet plan and instructions to follow after the surgery. You will be advised to take medication to reduce the amount of acid produced by your stomach for the first 3 months. You will also need to start taking multi-vitamins which will continue for life.
